Yello, death doula hotline, whatcha wanna know?
As we’re all settling into this space together, I feel like it’s a good time to answer some baseline curiosities that I’ve been asked over the years from the homies and beyond.
Welcome to my first edition of Ask a Death Doula!, where I answer your questions- the simple, the personal, and the weeird.
To submit a question, please click below and I’ll address these questions in future letters.
In case you missed it, I have already answered the two most frequently asked questions (What is a death doula? & How does a death doula do this?) in my welcome letter so check it out if these questions interest you.
Otherwise, here are a few more comin atcha!
How/why did you get into this work?
Simply, a very good and woke friend of mine named Laryssa told me of the existence of the death doula in 2020 and Boom! I lit up and ate up everything that the internets had to say about the profession. It all spoke to me in the form of multiple hell yesses so “when you’re called, you go” – an appropriate mantra for this line of work.
I don’t know what’s on the other side of death but what I do know is that a lot of the unimportant stuff that life likes to build up and calcify falls away during the end of someone’s life, and I like this.
While most people see death as an ending where time and space are closing down, I’ve always seen it as a rich time where space and love open up.
It’s a time where roles may reverse – parents/uncles/aunties are the ones being cared for, children become the carers. The values of self-sufficiency, independence, and having the will to fight an illness that were once praised and rallied behind are now being surrendered to the values of communal care, generosity, gratitude, and acceptance.
Everything feels a bit upside down and very few are equipped or prepared for this. There’s a lot of richness of love here but not many can see it because they’re distracted by the discomfort, the unfamiliar tasks, the anticipatory grief, and the healthcare system that is not set up to support families in this way.
I do this work because there is a better way of doing things and we intuitively know this to be true.
Our loved one is dying. We want you as our death doula. What are the immediate next steps?
Every family is different but here is an example of a more common scenario.
A loved one’s health has shifted and they’re saying they have weeks to months left.
After an initial call to answer any immediate questions and once I have a basic understanding of what’s happening, the next step would be for me to come visit the loved one and family wherever they are, typically at home or at the hospital.
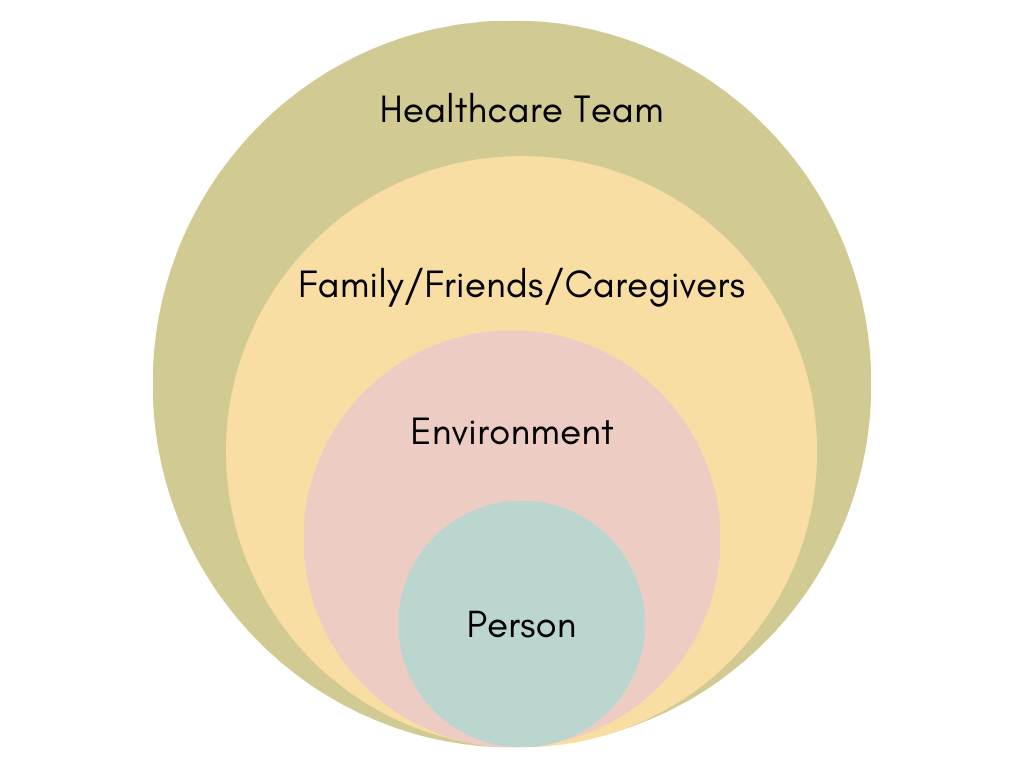
It’s during this time that I would meet the loved one dying and I’ll check in with them. I will assess their spirit, their physical body, where they are on their journey, how they want to be cared for, their wishes, their comfort level, etc. and communicate what I see and hear with the family. This is often a pivotal time where I’ll share with the family and caregivers what the person dying may be experiencing and how to best soften and support their journey at this moment.
From there, I’ll move outward and assess the environment around them. Together with the loved one and family, we will adjust the environment to make it familiar and more conducive to comfort, safety, and ease. Those that enter will know to tread lightly and softly.
Then, I’ll move outward into assessing how the family/friends/caregivers are. I’ll check in to see what kind of practical arrangements I can help with (finding the right hospice, advising on medical equipment, etc.) and whether I can assist in caregiver training for home care. More importantly, I’ll check in with the family/friends on how they are being cared for and how we can better take care of each other. This is typically reflected in a vigil plan which we would create together with the goals of communal care and in line with honoring the loved one’s wishes who is dying.
Lastly, I’ll check in with the healthcare and hospice team to ensure everyone is on the same page about the care plan moving forward with the appropriate values and quality of life for the loved one leading the way.
This is a comprehensive example of how the work can look. Of course, I’d prefer to complete this type of planning with you without a prognosis of weeks to months but alas, this is how it happens sometimes. More on the importance of end of life pre-planning in future letters!
For all us visual learners and chart geeks, I’ve put together this simple yet colorful peacock feather for your delight.
How do you separate yourself from the heaviness that death can carry?
Yea. I’ve experienced a few times where I’ve felt quite heavy when coming home after leaving families. In these times, I’ve found that either I’m physically exhausted, I’m giving myself a hard time around what the experience should be, or I’ve unknowingly taken on the heaviness of others. It happens.
When I’m physically exhausted, let’s say, after supporting a family with an overnight shift, afterwards, I’ll immediately take a shower, eat, and sleep. It’s simple and basic but those three things are what heal me most physically. It’s like if hangry took over the entire body. Just do the thing to temper the beast because if not, the mind will take offense and spin out as well.
If I’m giving myself a hard time around what I think the experience should be, I remind myself of the exact thing I’m trying to offer families: open and relax. What typically helps is when I can wisely and kindly tell myself “This isn’t about you” and then focus my energy and well wishes back on the person who is laboring through death. This refocusing usually opens my heart and relaxes it in a way to allow the experience to be what it is and ensures that my intentions are of good will.
If I find myself taking on the heaviness of others, I typically reach out to a trusted friend or family member for some much needed perspective and clarity. I’ll also sit and meditate to examine and begin to clear out what isn’t necessary.
These modes of healing are all works in progress but I’ve found them to be good friends that have really helped me along the way.
A last note. When it comes to being with someone who is dying, I often see someone that needs someone to soften their experience. Someone to translate their experience to their family. Someone to let them know that everything is going to be okay and that everything they’ve done in their life was more than enough. This I don’t find heavy. I find it to be quite cool. If anything, it brings light.
That’s what I got, folks. 🙂
Again, if you have any questions you’d like to submit, hit the button below!
Be happy,
Erika
